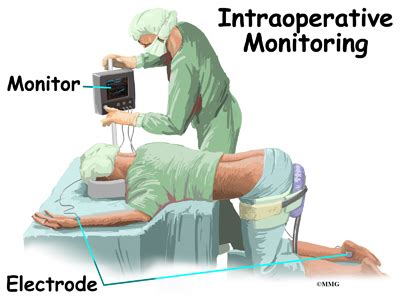
Intraoperative monitoring (IOM) technology has revolutionized the way surgical teams approach complex procedures. By providing real-time feedback on a patient's vital signs and physiological responses, IOM tech helps anesthesiologists and surgeons make data-driven decisions that can mean the difference between life and death. In this article, we'll explore seven ways IOM technology saves lives in the operating room.

1. Real-Time Vital Sign Monitoring
IOM technology allows for continuous, real-time monitoring of a patient's vital signs, including heart rate, blood pressure, oxygen saturation, and respiratory rate. This information is crucial in detecting any sudden changes or anomalies that may indicate a life-threatening complication.
How it saves lives:
- Enables prompt intervention in case of cardiac arrest or other emergencies
- Helps anesthesiologists adjust anesthesia levels to maintain stable vital signs
- Facilitates timely identification of postoperative complications, such as bleeding or respiratory distress
2. Electrophysiological Monitoring
Electrophysiological monitoring involves the use of EEG, EMG, and other modalities to assess the nervous system's function during surgery. This type of monitoring is particularly useful in neurosurgical procedures, where even slight deviations in neural activity can have significant consequences.

How it saves lives:
- Helps surgeons avoid damaging critical neural structures during dissection
- Enables real-time assessment of brain function, reducing the risk of cerebral damage
- Facilitates prompt intervention in case of seizures or other neurologic emergencies
3. Anesthesia Depth Monitoring
Anesthesia depth monitoring involves the use of various technologies, such as bispectral index (BIS) or entropy, to assess the level of consciousness during general anesthesia. This information helps anesthesiologists ensure that the patient is adequately anesthetized, reducing the risk of recall or other complications.
How it saves lives:
- Minimizes the risk of anesthesia awareness, a condition where patients recall surgical events
- Helps anesthesiologists adjust anesthesia levels to maintain optimal depths
- Reduces the risk of postoperative cognitive dysfunction (POCD)
4. Cardiac Output Monitoring
Cardiac output monitoring involves the use of technologies, such as pulse contour analysis or transpulmonary thermodilution, to assess the heart's pumping efficiency during surgery. This information is crucial in detecting any changes in cardiac function that may indicate a life-threatening complication.

How it saves lives:
- Enables prompt intervention in case of cardiac arrest or other emergencies
- Helps anesthesiologists adjust fluid management and vasopressor therapy to maintain optimal cardiac function
- Facilitates timely identification of postoperative cardiac complications, such as myocardial infarction or heart failure
5. Respiratory Function Monitoring
Respiratory function monitoring involves the use of various technologies, such as capnography or spirometry, to assess the lungs' function during surgery. This information is crucial in detecting any changes in respiratory function that may indicate a life-threatening complication.
How it saves lives:
- Enables prompt intervention in case of respiratory arrest or other emergencies
- Helps anesthesiologists adjust ventilation strategies to maintain optimal respiratory function
- Facilitates timely identification of postoperative respiratory complications, such as pneumonia or acute respiratory distress syndrome (ARDS)
6. Hemodynamic Monitoring
Hemodynamic monitoring involves the use of various technologies, such as arterial waveform analysis or pulse oximetry, to assess the cardiovascular system's function during surgery. This information is crucial in detecting any changes in blood pressure or cardiac output that may indicate a life-threatening complication.

How it saves lives:
- Enables prompt intervention in case of hypotension or other cardiovascular emergencies
- Helps anesthesiologists adjust fluid management and vasopressor therapy to maintain optimal blood pressure
- Facilitates timely identification of postoperative cardiovascular complications, such as bleeding or cardiac tamponade
7. Multimodal Monitoring
Multimodal monitoring involves the use of various technologies to assess multiple physiological parameters simultaneously. This approach enables anesthesiologists to gain a comprehensive understanding of the patient's physiological state, facilitating more informed decision-making.
How it saves lives:
- Enables prompt intervention in case of multiple organ dysfunction syndrome (MODS) or other emergencies
- Helps anesthesiologists adjust treatment strategies to maintain optimal physiological function
- Facilitates timely identification of postoperative complications, such as sepsis or multiple organ failure






In conclusion, intraoperative monitoring technology plays a vital role in ensuring patient safety during surgery. By providing real-time feedback on various physiological parameters, IOM tech enables anesthesiologists and surgeons to make data-driven decisions that can mean the difference between life and death. As technology continues to evolve, we can expect even more advanced monitoring systems to emerge, further improving patient outcomes and saving lives.
What is intraoperative monitoring?
+Intraoperative monitoring (IOM) refers to the use of various technologies to monitor a patient's physiological parameters during surgery.
What are the benefits of intraoperative monitoring?
+The benefits of IOM include improved patient safety, reduced risk of complications, and enhanced surgical outcomes.
What types of monitoring are used in intraoperative monitoring?
+Common types of monitoring used in IOM include electroencephalography (EEG), electromyography (EMG), cardiac output monitoring, and respiratory function monitoring.